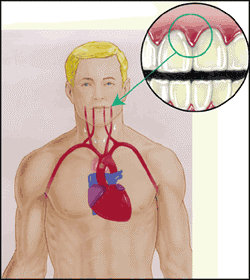
There is a strong connection between oral and systemic health. Increasing evidence points to a healthy mouth as a key indicator of overall health. Periodontal disease, or infection of the gums, is a disease of inflammation, as are many systemic diseases such as diabetes, heart disease, and osteoporosis. Though this inflammatory condition occurs in the mouth, it can affect the rest of the body, as the mouth is not independent from the rest of the body. Everything is connected .
Recent research reveals that gum disease is linked to increased risk for major overall health problems, including but not limited to stroke, heart disease, respiratory problems, osteoporosis, diabetes complications, low birth weight, and most recently, dementia. Because of these findings, research continues. We will probably learn much more in the next few years.
It does make perfect sense – gum disease linked to overall health problems. Everything that enters or is present in the mouth has access to the whole body. The mouth is a portal to the body. That’s why regular dental checkups and oral hygiene visits are vital to not only your oral health, but to your overall health as well.
One out of every two American adults over 30 has periodontal disease, according to recent findings from the Centers for Disease Control and Prevention (CDC). A study titled Prevalence estimates that 47.2 percent, or 64.7 million American adults, have mild, moderate or severe periodontitis, the more advanced form of periodontal disease. In adults 65 and older, prevalence rates increase to 70.1 percent. This study is published in the Journal of Dental Research, the official publication of the International and American Associations for Dental Research.
Periodontal disease is a chronic inflammatory disease that affects the gum tissue and bone supporting the teeth, according to the American Academy of Periodontology (AAP). If left untreated, periodontal disease can lead to tooth loss. Research has also shown that periodontal disease is associated with other chronic inflammatory diseases, such as diabetes and cardiovascular disease.
- Heart Disease
- Stroke
- Diabetes
- Obesity
- Pregnancy and Low Preterm Birthweight
- Osteoporosis
- Cancer
- Respitory Disease
- Chronic Kidney Disease
- Prostate Health
- Impotence
- Mild Cognitive Impairment
- Alzheimer’s Disease
- Rheumatoid Arthritis
HEART DISEASE
Several studies have shown that periodontal disease is associated with heart disease. Research has indicated that periodontal disease increases the risk of heart disease.
Scientists believe that inflammation caused by periodontal disease may be responsible for the direct link between heart disease and gum disease. Destruction of the gums resulting from periodontal disease allows oral bacteria to get into the bloodstream. This leads to inflammation which is responsible for the laying down of plaques in the blood vessels. Bacteria from the mouth has been found living in the plaques of blocked heart vessels.
Periodontal disease can also exacerbate existing heart conditions. Patients at risk for infective endocarditis may require antibiotics prior to dental procedures. We work with your cardiologist to be able to determine if your heart condition requires use of antibiotics prior to dental procedures.
STROKE
Additional studies have pointed to a relationship between periodontal disease and stroke. In one study that looked at the causal relationship of oral infection as a risk factor for stroke, people diagnosed with acute cerebrovascular ischemia were found more likely to have an oral infection when compared to those in the control group. Doesn’t that say something?
A national study conducted by the CDC found that people over 60 years old who have periodontal disease were more likely to have experienced a stroke. Patients with periodontal disease are 1.5-2.5 times more likely to suffer a stroke.
DIABETES
Diabetic patients are more likely to develop periodontal disease, which in turn can increase blood sugar and diabetic complications.
People with diabetes are more likely to have periodontal disease than people without diabetes, probably because people with diabetes are more susceptible to contracting infections. In fact, periodontal disease is often considered a complication of diabetes. Those people who don't have their diabetes under control are especially at risk.
Research has suggested that the relationship between diabetes and periodontal disease goes both ways - periodontal disease may make it more difficult for people who have diabetes to control their blood sugar.
Severe periodontal disease can increase blood sugar, contributing to increased periods of time when the body functions with a high blood sugar. This puts people with diabetes at increased risk for diabetic complications.
OBESITY
Obesity is excessive fat accumulation that poses a risk to health. Obesity is currently a worldwide health problem with over 500 million obese adults. Obesity also puts one at risk of developing other health problems such as Diabetes.
Studies have shown a strong association between obesity and periodontal disease.
PREGNANCY AND LOW BIRTH WEIGHT BABIES
Pregnant women who have periodontal disease may be more likely to have a baby that is born too early and too small. All infections are cause for concern among pregnant women because they pose a risk to the health of the baby. It is recommended that women considering pregnancy have a dental checkup and teeth cleaning before and while pregnant, and again after the baby is born, due to the effects of hormonal changes during pregnancy. We can help you minimize red, bleeding gums, dental pain and other health problems to lower the risk of infection causing low birth weight, premature babies and other complications.
OSTEOPOROSIS
Researchers have suggested that a link between osteoporosis and bone loss in the jaw. Studies suggest that osteoporosis may lead to tooth loss because the density of the bone that supports the teeth may be decreased which means the teeth no longer have a solid foundation.
Patients losing bone density from osteoporosis also show increased bone loss around their teeth. However, patients undergoing hormone replacement therapy and calcium and vitamin D supplementation for osteoporosis also showed improvement in their periodontal health and lost less teeth over time.
CANCER
Patients with periodontal disease show an increased risk in developing oral cancer, especially if they smoke or use alcohol. Patients with periodontal disease also appear to be at higher risk for lung, kidney, pancreatic, and haematological cancers.
Research has found that men with a history of gum disease are 14 percent more likely to develop cancer than men with healthy gums. Specifically, men with periodontal disease may be 49 percent more likely than women to develop kidney cancer, 54 percent more likely to develop pancreatic cancer, and 30 percent more likely to develop blood cancers.
RESPIRATORY DISEASE
Research has found that bacteria that grow in the oral cavity can be aspirated into the lungs to cause respiratory diseases such as pneumonia, especially in people with periodontal disease. People with poor oral health are at higher risk for developing pneumonia. Studies have calculated that one in ten deaths from pneumonia among the elderly in hospitals and nursing homes could be avoided by improving oral hygiene.
Chronic Obstructive Pulmonary Disease (COPD) is the sixth leading cause of death in the world. People with (COPD) are more likely to have periodontal disease. Smokers with (COPD) are three times more likely to have periodontal disease. The greater severity of gum disease, the greater the loss of lung function.
CHRONIC KIDNEY DISEASE
Chronic kidney disease is a long term reduced function of the kidneys from kidney damage. It is generally associated with diabetes, high blood pressure, obesity, cardiovascular disease, and ageing. Most of these risk factors are also associated with gum disease.
Studies have found patients with gum disease to be at increased risk for chronic kidney disease.
PROSTATE
Prostate-specific antigen (PSA) is an enzyme created in the prostate that is normally secreted in very small amounts. However, when the prostate becomes inflamed, infected, or affected by cancer, PSA levels rise. Research has shown that men with indicators of periodontal disease such as red, swollen or tender gums as well as prostatitis (inflammation of the prostate) have higher levels of PSA than men with only one of the conditions. This means that prostate health may be associated with periodontal health, and vice versa.
IMPOTENCE
Men with periodontal disease, especially those younger than 30 or older than 70, are at increased risk of developing impotence, according to research. Men in their thirties with gum disease are threee times more likely to suffer from erection problems. Researchers believe that inflammation may be the link between the two conditions; prolonged chronic inflammation (the same type of inflammation that is associated with periodontal disease) can damage blood vessels leading to impotence.
Seeing our hygienest regularly may help you in achieving and maintaining an erection.
MILD COGNITIVE IMPAIRMENT
Mild cognitive impairment is a decline in cognitive abilities greater than expected by ageing, but doesn’t interfere with daily life activities. Gum disease has been shown to be associated with mild cognitive impairment.
Patients who display mild cognitive impairment and also have complaints about memory are at much greater risk of developing Alzheimer’s Disease.
ALZHEIMER’S DISEASE
People with gum disease may be at greater risk of developing Alzheimer’s disease.
A component of oral bacteria associated with gum disease has been found in the brains of Alzheimer’s disease patients, but was not seen in the brains of healthy patients. The presence of this bacteria triggers the immune system in the brain which then leads to the death of neurons. This could be responsible for symptoms of Alzheimer’s disease such as confusion and memory loss.
Since we have no effective treatment for dementia and Alzheimer’s Disease, controlling risk factors for developing these conditions is very important.
RHEUMATOID ARTHRITIS
Patients with Rheumatoid Arthritis are eight times more likely to have periodontal disease. Oral bacteria have been found in the joints of rheumatoid arthritis patients. This leads to inflammation which is responsible for the destruction of bone and cartilage in the joints.
Treatment of gum disease has a positive impact on the control of Rheumatoid Arthritis severity. A clinical trial has found that conservative treatment for gum disease resulted in reduction of Rheumatoid Arthritis symptoms over a 6 week period.
TREATMENT FOR PERIODONTAL DISEASE
Treatment for gum disease is attempted to be accomplished in the most conservative means possible.
Initial treatment usually consists of scaling and root planning, also known as a deep cleaning. This is a very careful and thorough cleaning to remove the bacterial plaque and calculus buildup from the periodontal pockets under the gums. This may be combined with local delivery of medicine into the pockets.
After a six week healing period, the condition of the gums will be re-evaluated by a gum specialist.
Often, a deep cleaning combined with excellent home care is enough to achieve a state of periodontal health. If further active treatment is needed, that will be determined and discussed with the gum specialist.
MAINTENANCE
Since periodontal disease is a chronic, genetic condition, regular cleaning with a dental hygienest is a critical component in maintaining the gums in a healthy state. Research shows that patients with gum disease, who do not smoke and see their hygienest for cleanings every 3 months, rarely ever need to have active periodontal therapy repeated.
Back to Top ↑